Polycystic Ovary Syndrome
Polycystic Ovary Syndrome or (PCOS) is one of the most common endocrine conditions in reproductive aged women (ages 15-44), affecting 8-13% of women. It is believed that there could be as many as 1 in 5 of us affected.
What is PCOS? A hormonal condition. It involves cysts in the ovaries, high levels of male hormones, and irregular periods
PCOS affects a woman’s ovaries, the reproductive organs that produce estrogen and progesterone — hormones that regulate the menstrual cycle. The ovaries also produce a small amount of male hormones called androgens.
The ovaries release eggs to be fertilized by a man’s sperm. The release of an egg each month is called ovulation. Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) control ovulation. FSH stimulates the ovary to produce a follicle — a sac that contains an egg — and then LH triggers the ovary to release a mature egg.
PCOS is a “syndrome,” or group of symptoms that affects the ovaries and ovulation. Its three main features are:
Absent or irregular periods (amenorrhoea/oligomenorrhoea)
Signs of excess male hormones (including excess body or facial hair 'hirsutism', acne or high levels of these hormones 'hyperandrogenism' on a blood test)
Polycystic ovaries seen on an ultrasound scan (>12 follicles or 'cysts' in either ovary, follicles 2-9mm, ovarian volume >10mL)
In PCOS, many small, fluid-filled sacs grow inside the ovaries. The word “polycystic” means “many cysts.” These sacs are actually follicles, each one containing an immature egg. The eggs never mature enough to trigger ovulation. The lack of ovulation alters levels of estrogen, progesterone, FSH, and LH. Estrogen and progesterone levels are lower than usual, while androgen levels are higher than usual. Extra male hormones disrupt the menstrual cycle, so women with PCOS get fewer periods than usual.
Symptoms
Women with PCOS may experience:
infertility - problems getting pregnant (because of irregular ovulation or failure to ovulate), A lack of ovulation prevents the uterine lining from shedding every month. Some women with PCOS get fewer than eight periods a year
weight gain, up to 80 percent of women with PCOS are overweight or obese
thinning hair and hair loss
acne, male hormones can make the skin oilier than usual and cause breakouts on areas like the face, chest, and upper back
depression or mood changes
excessive hair growth (hirsutism). More than 70 percent of women with this condition grow hair on their face and body — including on their back, belly, and chest.
heavy bleeding. The uterine lining builds up for a longer period of time, so the periods you do get can be heavier than normal
darkening of the skin. Dark patches of skin can form in body creases like those on the neck, in the groin, and under the breasts.
headaches
What causes PCOS?
Until today doctors don't know exactly what causes PCOS. We know that high levels of male hormones prevent the ovaries from producing hormones and making eggs normally. Research has shown that PCOS is caused by a combination of our in-built genetics, epigenetics (how our genes are turned on and off), environmental factors and how we live our lives.
Diagnosing PCOS
The diagnosis and treatment of PCOS remains controversial and with many challenges. Up to 70% of affected women do not know they have PCOS and remain undiagnosed.
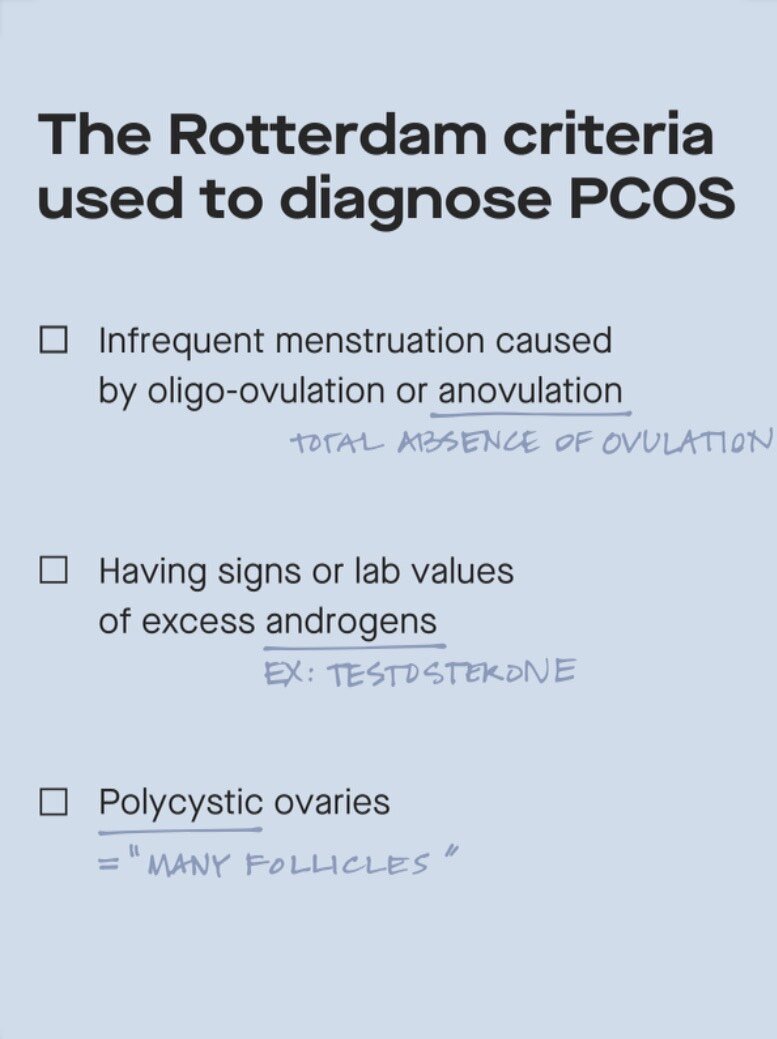
The Rotterdam criteria are the most widely accepted for PCOS diagnosis and the national guidelines reference these criteria. Women with 2 out of 3 of these criteria are diagnosed with PCOS.
Fertility Talk Dictionary
Amenorrhea: no menstrual period >3 months
Oligomenorrhoea: Infrequent menses. Menstrual cycles lasting >42 days or ≤ 5 menses per year
Insulin resistance
One key feature of PCOS is insulin resistance and found in over 70% of PCOS sufferers. In insulin resistant PCOS, the body is able to make plenty of insulin but tissues are less sensitive to it, forcing the body to produce more and more insulin.
Insulin- What is it? A key hormone responsible for keeping blood sugars under control
This high level of insulin then forces the ovaries to convert estrogen to the male hormone testosterone which halts ovulation.
What does this mean? A reduction in estrogen and increase in testosterone means no ovulation, no periods, acne, excess air, mood swings and often times difficulty conceiving or infertility.
Increased insulin = conversion of estrogen to testosterone
For those who do not fall under the category of insulin resistant (30% of those with PCOS) there are other causes. The adrenal glands produce testosterone in addition to cortisol, noradrenaline and adrenaline which can result is PCOS.
Management
There is no cure for PCOS but there are plenty of ways to improve symptoms
1. Lifestyle Interventions
Lifestyle modifications are the first line treatment for PCOS and they can reduce the risk of a lot of long term health consequences.
Weight loss:
Moderate weight loss of 5-10% can restore ovulation. Losing fat is one of the most effective ways to help the symptoms of PCOS, losing fat reduces insulin resistance which is the main driver of the condition. Losing weight can restore ovulation, reduce acne and reduce the risk of diabetes and heart disease in the future.
Exercise:
Consistency is key when it comes to exercise so it's best to find what you like - and what you will stick to. Altering body composition to increase lean muscle and reduce fat has been shown to improve PCOS symptoms as insulin is more sensitive to muscle. In adults from 18 – 64 years, a minimum of 150 min/week of moderate intensity physical activity or 75 min/week of vigorous intensities or an equivalent combination of both, including muscle strengthening activities on 2 non-consecutive days/week are advised.
Diet:
Eating carbohydrates - the right types carbohydrates - is very important for women with PCOS. A high fibre good quality diet that includes foods such as oats, brown rice, fruits and veggies are key. These foods are packed with all the necessary nutrients the body needs for all of the complex chemical processes such as ovulation. Health fats are also very important as all hormones are based upon these fats (cholesterol). 'If you don't have the building blocks you can't make the goods.'
Relaxation
Self care is so important in women with PCOS. Women with PCOS are already at an increased risk of anxiety and depression. Stress results in an increase in cortisol with increases insulin resistance and testosterone levels and so making time for self care is crucial.
2. Medication
Letrozole - ‘Femara’ (first line)
A few years ago, a Cochrane systematic review reported that Letrozole (brand name Femara) had a 44% higher pregnancy rate thank Clomid for PCOS women, but the quality of the evidence wasn’t convincing at the time. More recently, a recent study with a much better design has tried to answer the question: which is a better first line ovulation induction method for anovulatory PCOS women -- Clomiphene Citrate (Clomid) or Letrozole (Femara)? They compared ovulation rates, pregnancy, live birth, and more. Femara looked much better than Clomid on just about every meaningful outcome.
Combined Oral Contraception
Inositol, in the form of myo-inositol, may help improve fertility rates in women with polycystic ovarian syndrome (PCOS). Inositol has been shown to help modulate the presence of insulin in the body, which may have significant effect on ovulation. This helps improve glucose metabolism in women with PCOS. Clinical studies have demonstrated that Inositol can help restore normal ovulation, improve egg quality and increase fertilization rates in women with PCOS. For example, a 40 : 1 ratio between myo-inositol and D-chiro-inositol is the optimal combination to restore ovulation in women with PCOS, due to their combined impacts on blastocyst quality, intestinal absorption, and impact on androgen levels.
Long term health consequences of PCOS
There are several long term health consequences that women with PCOS should be aware of.
Reproductive Health: Menstrual irregularities which can cause infertility.
Metabolic Health: Insulin resistance, obesity, impaired glucose tolerance, type 2 diabetes, dyslipidemia can all increase the risk for cardiovascular disease.
Cancer: Women with polycystic ovarian syndrome have a 2-6 fold increased risk for developing endometrial cancer (cancer of the lining of the uterus). A major factor for this increased malignancy risk is prolonged exposure of the endometrium to unopposed estrogen that results from no ovulation (anovulation).
Therefore it is very important to look out for these signs and symptoms and get checked with your gynecologist if you have any concerns or above mentioned signs or symptoms.
Resources:
Have a question for us? Feel free to leave a comment below or alternatively, submit your questions through our contact/subscription page.