What is Ovarian Reserve?
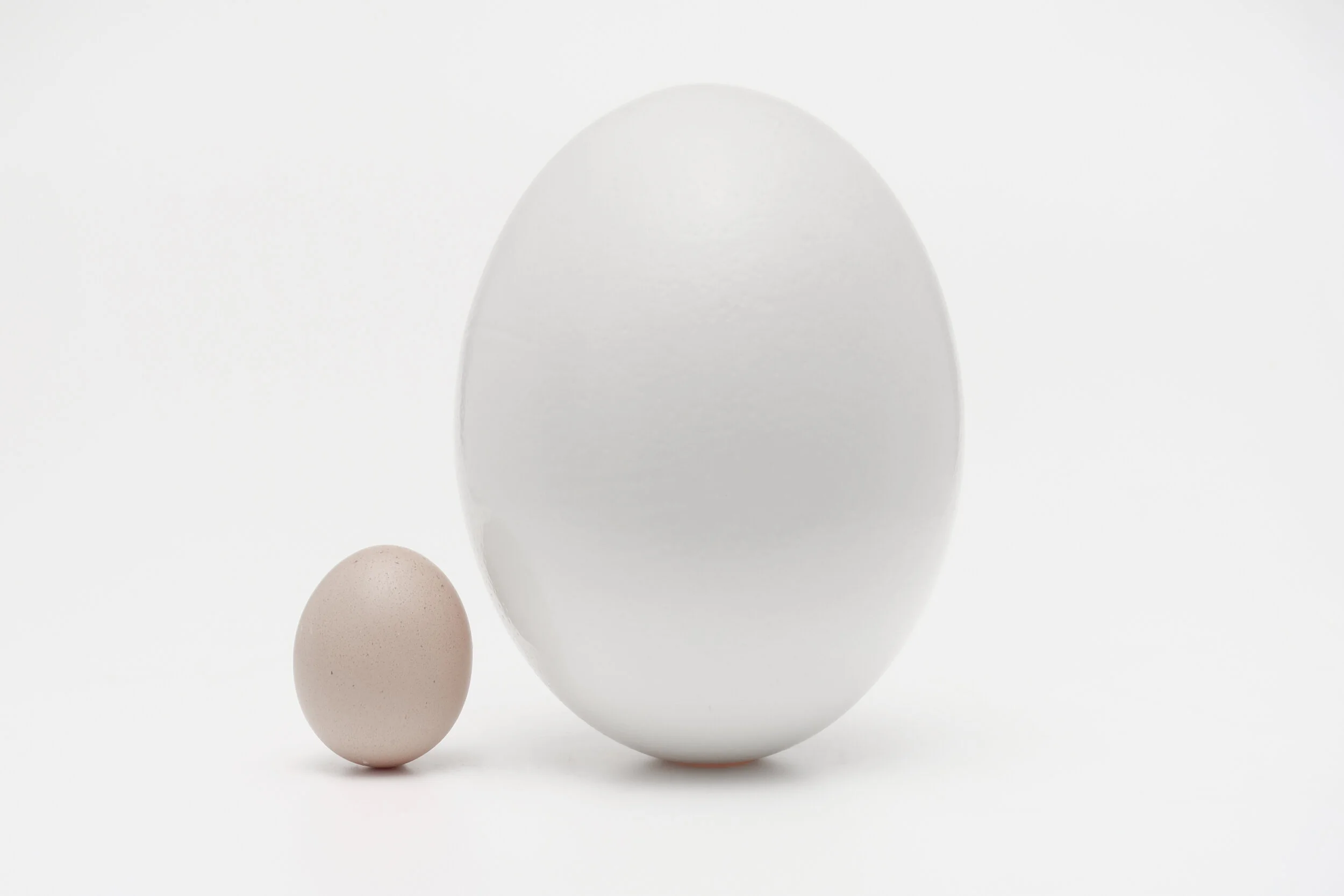
Let's talk ovarian reserve. The quantity of eggs that are within the ovaries.
But first... let’s get back to basics to understand how it all works.
Fun Fact
Did you know your grandmother carried a part of you inside her womb?
But how? Well…
A female fetus is born with all the eggs she will ever have in her lifetime. So when your Grandmother was carrying your Mother in her womb you were tiny eggs in your Mother’s ovaries.
The three of you have been connected for a very long time.
When we are growing in our mother’s tummy at between 18-22 weeks our ovaries contain their peak number of egg cells (approx 7 million). By the time we are born this number has reduced to 2 million and by puberty to approx 300,000. Consider this your ‘egg reserve’. Once you hit puberty around age 13, the ovary releases one egg every month through ovulation. If fertilised by a sperm pregnancy may occur and if not - a period. I know what you're thinking, and if you're better at math than me...surely this means that if we have our period at age 13 and release one egg per month then we should have plenty of eggs to last a lifetime?! Well not quite. Many other eggs die off in a process called ‘atresia’ every month (around 1,000) alongside your egg that ovulates and so our reserve is depleted each year until we reach menopause at age 51 (average).
Let's Talk Technical: What is Atresia? The degeneration of those ovarian follicles which do not ovulate during the menstrual cycle
If you are interested to know your ovarian reserve, your doctor can do a transvaginal ultrasound (counting the antral follicles 'eggs') and also order the following blood tests:
anti-Mullerian hormone 'AMH'
follicle stimulating hormone 'FSH'
leutenizing hormone 'LH'
estradiol 'E2'
inhibin-B
Explain Please?
AMH is a hormone secreted by the granulosa cells of each dormant and growing follicle (egg), and a very good indicator of a woman's ovarian reserve. With very little variation throughout a woman's cycle, this test can be done at any time.
FSH hormone stimulates the growth of ovarian follicles in the ovary and is produced by the pituitary gland in the brain. This test must be done between cycle day 2-4 and can fluctuate from month to month.
LH hormone is secreted by the brain and promotes growth of a follicle and is responsible for ovulation. It is best measured on cycle day 2-4.
Estradiol hormone is a form of Estrogen and the primary female sex hormone. Also done between day 2-4 of the cycle, this hormone acts as a growth hormone for tissue of the reproductive organs, supporting the lining of the vagina, the cervical glands, the endometrium and the lining of the fallopian tubes. It's also crucial for egg growth and ovulation.
Inhibin-B is a hormone secreted by the ovaries. FSH stimulates the growth of a follicle. Inhibin secretion increases from the ovaries after an egg ovulates, suppressing FSH production so another egg does not grow (hoping a pregnancy will occur).
The higher the level of AMH in the blood, the higher the ovarian reserve and a good indicator of your fertility potential. A high AMH can also indicate Polycystic Ovary Syndrome (PCOS).
The higher the FSH however, the harder the body is having to work to produce an egg...not a good sign. High levels of FSH and estradiol can indicate low egg quality and quantity and low levels of estradiol can indicate PCOS and hypopituitarism. It is normal for the AMH level to decline and FSH levels to increase as women get older. As the eggs are depleting, so too is the AMH level until the point of menopause.
Depending on your results your fertility doctor can advise you on your ovarian reserve and what is normal for your age? A low level does not mean you are unable to conceive so please remember this. Don't sweat the numbers! Everything should be discussed within context.
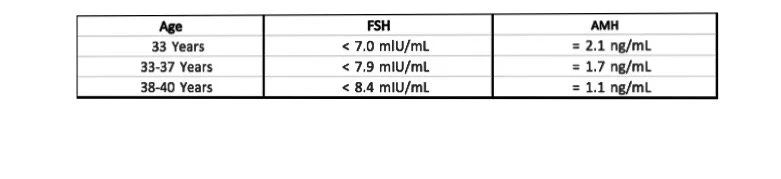
AMH and FSH range by Age (Cycle day 3 blood test)
Very low AMH is usually thought to be an AMH below 1.05 ng/ml, and undetectably low AMH levels are calculated as below 0.16 ng/ml. A low level of FSH can also be an additional indicator of a problem with the quantity of a woman’s eggs.
But I am on the oral contraceptive pill. Will the AMH test be accurate?
Research has shown that there can be a discrepancy of up to 30% for women who are on the oral contraceptive pill when doing this test. The OCP can suppress the AMH level and therefore provide you with a lower result. This is temporary of course while on the OCP and does not permanently effect the reserve or future fertility.
The Research
Kallio et al (Fertil Steril 2013) was the first to study this. He studied 42 healthy women over a period of nine weeks. Women had baseline blood hormone levels (AMH, Inhibin B, FSH, LH, E2) drawn and then were treated with hormonal contraceptives (13 women), patches (15 women) and vaginal ring (14 women). Blood levels were evaluated at 5 and 9 weeks later.
Get to the point...
All 5 hormones including AMH were significantly suppressed at 9 weeks. AMH levels (ng/mL) were 3.88+3.0 at baseline, 3.34+2.8 at 5 weeks and 1.91+1.5 at 9 weeks.
What does this mean?
Serum antimullerian hormone (AMH), FSH, inhibin B, LH, and E 2 levels had decreased significantly in all study groups after 9 weeks of treatment. The decrease in AMH was less than the others but still present and indicates that follicle growth is suppressed using these hormonal contraceptives.
The AMH test should be considered a screening test and used carefully in combination with other results to determine fertility potential (FSH levels, Estradiol and antral follicle count 'AFC'). Remember this test only indicates the quantity of eggs and not the quality of eggs....another very important factor to consider when talking about fertility. When going for these tests, make sure you are using a reputable accredited lab and an experienced doctor who can correctly interpret your results.
There is no test to check for egg quality
If going through fertility treatments, ovarian reserve results can allow your doctor to determine the protocol and hormonal stimulation best suited to you. It allows your doctor to anticipate the response you may have and egg numbers you may produce. It is only at the time of egg collection during fertility treatments when the egg quality can be assessed. This however will only assess the quality visible under microscope (cytoplasm, color and shape) and not the genetic make up of the egg (chromosomes).
The Debate: When should you perform this test?
There are lots of mixed opinions when it comes to routine AMH testing as a means of assessing fertility. The American College of Obstetricians and Gynecologists have advised that based on the current information, a single serum antimüllerian hormone level assessment obtained at any point in time in a population of women with presumed fertility does not appear to be useful in predicting time to pregnancy and should not be used for counseling patients in this regard. At this time, routine antimüllerian hormone testing for prediction of pregnancy loss is also not recommended. More data are needed to determine the utility of antimüllerian hormone as a predictor of time to menopause, a biomarker for polycystic ovary syndrome, or a predictor of future menses in women who have received gonadotoxic therapy (chemotherapy).
Let’s imagine a scenario:
Imagine, a 30 year old single lady with no known fertility problems performs this test. She has not yet started to plan for a family as she is pursuing higher education. Her result shows a low reserve level for her age and she finds herself in a dilemma. Let's hold it here.
This low level does not mean that she's unable to conceive now or in the coming years. As per ACOG, a single serum antimüllerian hormone level assessment obtained at any point in time in a population of women with presumed fertility does not appear to be useful in predicting time to pregnancy. It could however allow her to have a serious conversation with her gynecologist/fertility specialist about family planning (i.e when she plans to start a family) and other options available to her such as egg freezing, if she so wishes.
Now, imagine a 38 year old who receives an above average level for her age indicating she has a good ovarian reserve. There is a risk that this level can falsely reassure her that she shouldn't be thinking about family planning or fertility preservation (egg freezing). This level as we have said, does not reflect quality and therefore her eggs are technically 38 years old. There might be many of them, but many of them will have a higher rate of aneuploidy (abnormal genetics). Meaning less likely to produce a normal pregnancy. All women have some percentage of abnormal eggs. According to studies, women in their early 20s have about 20% abnormal eggs, while women in their 40s have upwards of 80% abnormal eggs. Meaning this lady may have difficulty conceiving a healthy baby with increasing difficulty as the years go on.
There might be many eggs, but many of them will be aneuploid (genetically abnormal)
While tests to check AMH and FSH levels are important in assessing ovarian reserve, both have limitations. Neither result can, indeed, categorically determine whether a woman can or cannot conceive, unless she has very high FSH levels. In addition, women can get pregnant with IVF even when AMH is completely undetectable. Although it cannot be considered as itself as a reliable predictor of pregnancy in women, AMH is now a useful tool in the management and treatment of female infertility, allowing doctors to predict ovarian response to exogenous gonadotropin stimulation in women undergoing assisted reproduction cycles (ie. IVF). If women do decide to use this test as part of a general fertility assessment, the benefits are that the results may prompt them to open the topic of family planning with their partners, something that in my opinion should be discussed as soon as possible if one wishes to have a family.
Listen to our Fertility Talk Podcast on ovarian ageing and fertility preservation where we talk more about these tests and if or when you should consider taking them.
Have a question for us? Feel free to contact us. Alternatively, you can find us on Instagram @thefertilitytalk