Corona Virus (COVID 19) and Your Fertility
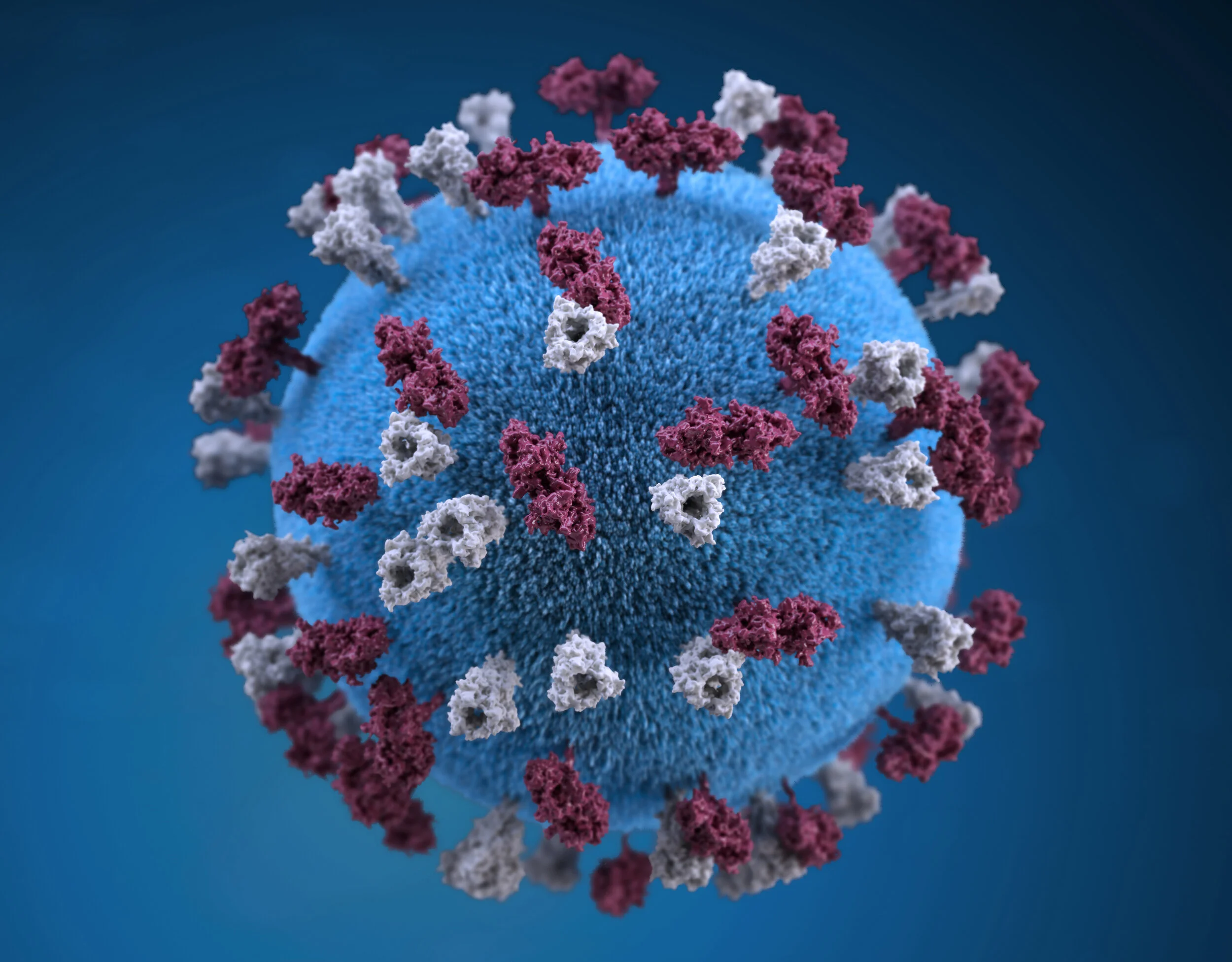
COVID-19 is a new illness that can affect your lungs and airways. It's caused by a virus called coronavirus.
For people who get infected with coronavirus:
80% will have mild illness and make a full recovery within a few weeks
14% will have a more severe illness
6% will have a critical illness
We are carefully following the coronavirus pandemic and global governmental measures that are being put in place to contain and mitigate the spread of the virus. We are monitoring updates issued by the The Royal College of Obstetrics, The Centre for Disease Control and Prevention (CDC), and the Human Fertilisation and Embryology Authority (HFEA). Please be aware that this is very much an evolving situation and this guidance, set out by varying authorities, is a living document that may be updated if or when new information becomes available. We therefore suggest that you visit this page as well as the CDC, WHO, RCOG regularly for any updates.
The consensus is that:
COVID-19 is a new disease and we are still learning how it spreads, the severity of illness it causes, and to what extent it affects fertility, pregnancy and newborns.
Is there a risk to pregnant women?
As per the CDC, they do not currently know if pregnant women have a greater chance of getting sick from COVID-19 than the general public nor whether they are more likely to have serious illness as a result. Pregnant women experience changes in their bodies that may increase their risk of some infections. With viruses from the same family as COVID-19, and other viral respiratory infections, such as influenza, women have had a higher risk of developing severe illness. It is therefore very important for pregnant women to protect themselves from illnesses.
How can pregnant women protect themselves from getting COVID-19?
Pregnant women should do the same things as the general public to avoid infection. You can help stop the spread of COVID-19 by taking these actions:
Cover your cough (using your elbow is a good technique)
Avoid people who are sick
Clean your hands often using soap and water or alcohol-based hand sanitizer
You can find additional information on preventing COVID-19 disease at CDC’s (Prevention for 2019 Novel Coronavirus).
Can COVID-19 cause problems for a pregnancy?
The CDC do not know at this time if COVID-19 would cause problems during pregnancy or affect the health of the baby after birth.
During Pregnancy or Delivery
Can COVID-19 be passed from a pregnant woman to the fetus or newborn?
The CDC still do not know if a pregnant woman with COVID-19 can pass the virus that causes COVID-19 to her fetus or baby during pregnancy or delivery. No infants born to mothers with COVID-19 have tested positive for the COVID-19 virus. In these cases, which are a small number, the virus was not found in samples of amniotic fluid or breastmilk.
Infants
If a pregnant woman has COVID-19 during pregnancy, will it hurt the baby?
The CDC do not know at this time if any risk is posed to infants of a pregnant woman who has COVID-19. There have been a small number of reported problems with pregnancy or delivery (e.g. preterm birth) in babies born to mothers who tested positive for COVID-19 during their pregnancy. However, it is not clear that these outcomes were related to maternal infection.
What is known about COVID-19 in pregnancy?
Currently, there is limited information from published scientific reports about the susceptibility of pregnant women to COVID-19 and the severity of infection. Available data are reassuring but are limited to small case series. In general, pregnant women experience immunologic and physiologic changes that make them more susceptible to viral respiratory infections, including potentially COVID-19. It is reasonable to predict that pregnant women might be at greater risk for severe illness, morbidity, or mortality compared with the general population, as is observed with other related coronavirus infections [including severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV)], and other viral respiratory infections, such as influenza, during pregnancy. Data from MERS-CoV and SARS-CoV, although limited, suggest that infection in pregnancy may be associated with severe infection and adverse neonatal outcomes, including increased risk of miscarriage, fetal growth restriction, and preterm birth. But again, data specific to COVID-19 are not yet available.
The currently published data on COVID-19 infection in pregnancy include 2 case series, totaling 18 women, only 1 of whom suffered severe respiratory morbidity requiring intensive care unit admission and mechanical ventilation (lower than the reported general population risk). The data showed that 19 babies were born (one se too twins) without contracting the virus. There was no intrauterine transmission (called vertical transmission). 16 of the 18 women delivered their babies via c.section and were all in their 3rd trimester when they contracted the virus. While these data are reassuring that pregnant women did not have severe outcomes, they must be interpreted with caution given the small numbers. At this time, it appears that severe illness from COVID-19 occurs predominantly among the elderly and those with significant medical comorbidities.
Does COVID-19 cause miscarriage or congenital anomalies?
At this time, very limited data regarding risks associated with infection in the first and second trimesters exist. There are mixed data regarding the risk of congenital malformations in the setting of maternal fever in general. Currently, there are inadequate data on COVID-19 and the risk of miscarriage or congenital anomalies. Data from the SARS epidemic are reassuring, suggesting no increased risk of fetal loss or congenital anomalies associated with infection early in pregnancy.
Breastfeeding
Interim guidance has been made available on the CDC website and is intended for women who are confirmed to have COVID-19 or are persons-under-investigation (PUI) for COVID-19 and are currently breastfeeding. This interim guidance is based on what is currently known about COVID-19 and the transmission of other viral respiratory infections. CDC will update this interim guidance as needed as additional information becomes available. For breastfeeding guidance in the immediate postpartum setting, refer to Interim Considerations for Infection Prevention and Control of 2019 Coronavirus Disease 2019 (COVID-19) in Inpatient Obstetric Healthcare Settings.
Transmission of COVID-19 through breast milk
Much is unknown about how COVID-19 is spread. Person-to-person spread is thought to occur mainly via respiratory droplets produced when an infected person coughs or sneezes, similar to how influenza (flu) and other respiratory pathogens spread. In limited studies on women with COVID-19 and another coronavirus infection, Severe Acute Respiratory Syndrome (SARS-CoV), the virus has not been detected in breast milk; however we do not know whether mothers with COVID-19 can transmit the virus via breast milk.
CDC breastfeeding guidance for other infectious illnesses
Breast milk provides protection against many illnesses. There are rare exceptions when breastfeeding or feeding expressed breast milk is not recommended. CDC has no specific guidance for breastfeeding during infection with similar viruses like SARS-CoV or Middle Eastern Respiratory Syndrome (MERS-CoV).
Outside of the immediate postpartum setting, CDC recommends that a mother with flu continue breastfeeding or feeding expressed breast milk to her infant while taking precautions to avoid spreading the virus to her infant.
Guidance on breastfeeding for mothers with confirmed COVID-19 or under investigation for COVID-19
Breast milk is the best source of nutrition for most infants. However, much is unknown about COVID-19. Whether and how to start or continue breastfeeding should be determined by the mother in coordination with her family and healthcare providers. A mother with confirmed COVID-19 or who is a symptomatic PUI should take all possible precautions to avoid spreading the virus to her infant, including washing her hands before touching the infant and wearing a face mask, if possible, while feeding at the breast. If expressing breast milk with a manual or electric breast pump, the mother should wash her hands before touching any pump or bottle parts and follow recommendations for proper pump cleaning after each use. If possible, consider having someone who is well feed the expressed breast milk to the infant.
The Guidelines If Going Through Infertility Treatments:
The American Society for Reproductive Medicine (ASRM) Guidelines:
Currently, very little is known about the impact of COVID-19 on reproduction and pregnancy. There are reports of women who have tested positive for COVID-19 delivering babies free of the disease. This data is reassuring but must be interpreted with caution given the small numbers. Other forms of coronavirus have been linked to increased adverse outcomes during pregnancy, but data specific to COVID-19 is not yet available. It should be emphasized, however, that coronaviruses are unrelated to the ZIKA virus, which had very clear implications for pregnancy and fetal development. Given the information we do have, while it would be wise for individuals with confirmed or presumed COVID-19 infection to avoid pregnancy, there appears to be no cause for alarm for those already pregnant.
Nonetheless, out of an abundance of caution, patients who have high likelihood of having COVID-19 (fever and/or cough, shortness of breath, and either exposure within 6 feet of a confirmed COVID-19 patient and within 14 days of onset of symptoms, or a positive COVID-19 test result), including those planning to use oocyte donors, sperm donors, or gestational carriers, should strive to avoid a pregnancy. If these patients are undergoing active infertility treatment, we suggest that they consider freezing all oocytes or embryos and avoid an embryo transfer until they are disease-free. It is important to note that this recommendation does not necessarily apply when there solely is a suspicion of COVID-19, because symptoms of COVID-19 are very similar to other more common forms of respiratory illnesses.
ASRM and SART remain concerned that travel restrictions due to the virus may cause intended parents who are using a gestational carrier not to be able to join their newborn in a timely manner. Consequently, they strongly encourage all intended parents and the legal professionals, organizations, and programs that facilitate these arrangements to promptly take the necessary steps to identify families that may be so affected and develop contingencies in the event that these babies need to be cared for following their birth.
Finally, it’s really important to stay abreast of new findings that emerge as a result of ongoing pregnancies and births.
2. The Human Fertilisation and Embryology Authority
The message from the HFEA is that patients who are currently undergoing fertility treatment or who are pregnant should contact their clinic for advice. Guidance issued by the Joint UK Blood Transfusion and Tissue Transplantation Services Professional Advisory Committee (JPAC) states:
Potential donors must not donate if:
a) Less than 28 days from a donor’s return from a Coronavirus risk area. This includes transit through an airport in a Coronavirus risk area, even if the traveller has not left the airport.
b) Less than 28 days from the last contact with a person with Coronavirus infection.
c) Less than 28 days since recovery from Coronavirus infection or possible Coronavirus infection.
We will collate information about any clinics that are affected to ensure we have an overview of the national fertility service provision throughout this pandemic and will update our information accordingly.
Take Home Message
Stay abreast of the latest guidelines and updates issued by the U.S. Centers for Disease Control and Prevention (CDC) and the U.S. Food and Drug Administration (FDA), the CDC, RCOG and HFEA websites regarding evolving developments concerning the COVID-19 pandemic.
Wash your hands often with soap and water for at least 20 seconds especially after you have been in a public place, or after blowing your nose, coughing, or sneezing.
If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
Avoid touching your eyes, nose, and mouth with unwashed hands.
Isolate yourself from anybody suspected of being infected with the Virus.
Avoid close contact with people who are sick.
Put distance between yourself and other people if COVID-19 is spreading in your community. This is especially important for people who are at higher risk of getting very sick
Stay home if you’re sick.
Do
keep a space of 2 metres (6.5 feet) between you and other people
reduce physical interactions with people
reduce the number of people you meet every day
avoid communal sleeping areas
avoid crowded places
work from home unless it is essential that you go to your workplace
Cover your mouth and nose with a tissue or your sleeve when you cough and sneeze.
Put used tissues into a bin and wash your hands.
Clean and disinfect frequently touched objects and surfaces.
Avoid close contact with people - keep a distance of 2 metres (6.5 feet) between you and others.
Avoid crowded places, especially indoors.
Avoid non-essential travel overseas and follow the DFA's travel advice.
Stay at home if you are sick to help stop the spread of whatever infection you may have.
Don't
do not shake hands or make close contact, if possible
Do not touch your eyes, nose or mouth if your hands are not clean.
Do not share objects that touch your mouth – for example, bottles, cups.
Please Note: All information in the above article is accurate at time of writing and publication (11th March 2020). Due to the evolving nature of the pandemic, it is advised to check directly with the sources available for the most up to date findings.
Have a question for us? Feel free to contact us. Alternatively, you can find us on Instagram @thefertilitytalk